Breast cancer is the most common cancer among women. Although great advances have been made in the early detection of this cancer, the need for removal of a major portion of the breast or the entire breast is still necessary for some of those who are afflicted with this disease. When the breast is removed, either partially or completely, the normal balance of the female chest is altered. This imbalance may be devastating to the patient. The psychological and physical trauma of breast cancer is a severe impediment to the normal lifestyle of a woman. Plastic surgeons are among a team of physicians that have helped women with breast cancer recover from this disease. A plastic surgeon can recreate a new breast in the case of complete breast removal or equalize the shape of the two breasts in the case of partial breast removal. This reconstruction greatly improves the overall shape and balance of the female chest and helps to lessen the psychological trauma of breast cancer.
Breast reconstruction is an operation designed to restore natural and symmetrical breasts to a woman who has had a partial or complete loss of a breast as a result of cancer trauma or congenital deformity.
With breast reconstruction, your Virginia plastic surgeon can restore the natural volume and symmetry of the breast. The patient may have lost one or both breasts. Sometimes, the cancer treatment is less destructive and only a portion of the breast is removed. In any case, the patient loses the natural shape and symmetry of her breasts. The loss of a breast for a woman is a traumatic event and has far-reaching psychological consequences. With breast reconstruction, the patient can achieve a more natural shape and achieve better symmetry between the breasts. Nipple areola reconstruction is the final stage of the breast reconstruction process. In this stage, the nipple and areola of the person who has had a mastectomy is restored. As a result of breast reconstruction, a woman with breast cancer can restore her body image and self-esteem and is better prepared to the deal with the devastating psychological consequences of having breast cancer.
In the first consultation, you will get a chance to discuss your concerns with our patient care coordinators and Dr. Marefat. The reconstructive options that are available to you will be discussed in detail. We will tell you what you need to know about your procedure and will help you determine what is best for you. You will receive information booklets, review before and after photographs, and receive pricing on the procedures.
The defect after your cancer operation will dictate the reconstructive method that can best restore your shape. The choices for breast reconstruction fall into 3 major categories. The first involves techniques that use an implant or prosthesis for reconstruction. The second are those techniques that use your own tissues (fat, muscle, skin) for reconstructing the breast. These procedures are called autologous breast reconstruction. The third combines the two procedures and uses implants as well as your own tissues. The choice of method depends on many variables. It is best to discuss these methods with Dr. Marefat.
After surgery, you may be admitted to the hospital for observation. Normally, the general surgeon doing your mastectomy or lumpectomy will be your admitting physician and will decide when you can go home. At least 1-2 days of hospitalization is to be expected. The recovery time will depend on the procedure(s) that you had done. In general, recovery is shorter for implant reconstruction.
The sutures for breast surgery are taken out in stages. Normally, we take some of the sutures out before a week. The rest of the sutures are taken out about 2-3 weeks after surgery.
We like to see our patients frequently after surgery. You are seen by the doctor or nurse within 2-3 days of surgery. Then, the normal routine is 1 week, 1 month, 3 months, 6 months, and 12 months after surgery. Of course, if there is a need, you are seen as many times as necessary. We encourage our patients to come for routine follow-up visits every 3-5 years.
You should be able to put makeup on your bruises after the first week. However, we do not recommend putting makeup on your incisions until they have completely healed because this may result in tattooing of the skin by the pigments of the makeup.
The ideal candidate for breast reconstruction is a person who is motivated to do what is necessary to get the best possible reconstruction of the breast. No result will be as natural as the breast before it was inflicted with cancer or had been operated on for cancer removal. You should have realistic goals and expectations. It is important not to compare your newly reconstructed breast with what you had before your mastectomy or lumpectomy. As plastic surgeons, we strive to get the best shape and symmetry possible. However, some degree of asymmetry is unavoidable. The less severe the deformity from your cancer operation is, the better your chances are to have a natural-looking breast after reconstruction. Generally, the younger you are, the better a candidate you are for surgery. But the physiological age of a person is more important than the chronological age. That is to say you may be 60 years old, but your skin and general health could be better than that of most 50 year olds.
This surgery should be covered by your insurance company. If you do not have insurance and want to have this procedure done, please see your plastic surgeon for an estimate of the cost of surgery.
If you do not have insurance, you can pay for breast reconstruction surgery by certified check, credit card, or cash. Payment for surgery is expected prior to the procedure. If you are having your surgery scheduled several weeks in advance, you can pay by personal check.
Yes. The extent of scarring will depend on the type of reconstruction performed. Some cancers are small and can be treated with a lumpectomy (removal of a part of the breast). In such cases, it is possible to reshape the breast with less scarring. On the other hand, if you are getting tissue from your abdomen or back for reconstructing the breast, you will not only have the scars on the breast but also have the scars on the abdomen or the back where tissue was taken. Most scars fade with time and become less visible, but they never go away completely.
Yes. However, the pain involved in breast reconstruction is very tolerable. We have heard our patients describe it as muscle aches and pain or just soreness. Many patients do not finish the pain medications prescribed to them for pain relief. But having said that, remember that pain is very subjective, and it is not easy to predict what degree of pain you will have.
No. Breast reconstruction is almost always done with the patient under general anesthesia. Minor procedures for adjustment of the breast, scar revisions, or parts of the nipple reconstruction may be done with sedation and local anesthesia.
The majority of breast reconstruction procedures are done in the hospital or ambulatory surgical center. When a procedure or touch-up is very simple and can easily be anesthetized, your surgeon may elect to do it in the office.
BEFORE
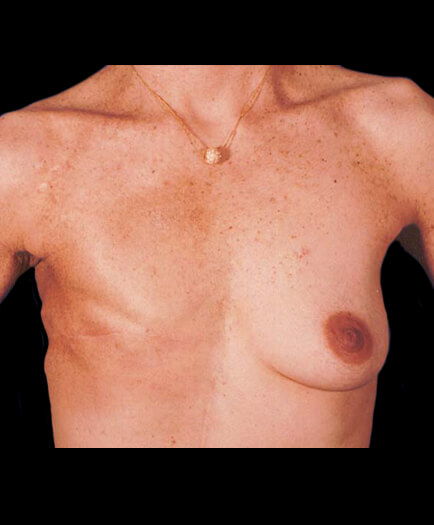
AFTER
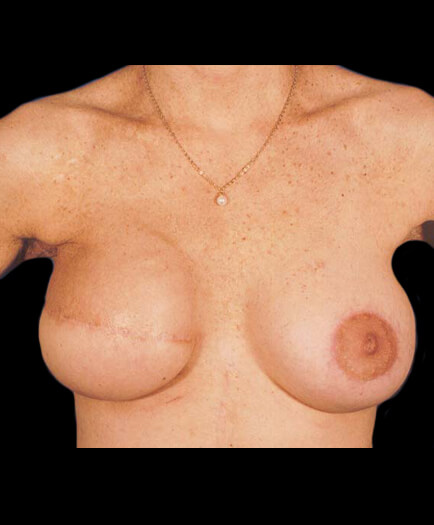
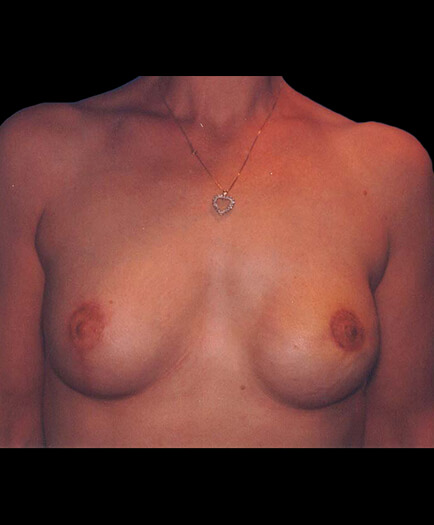
BEFORE
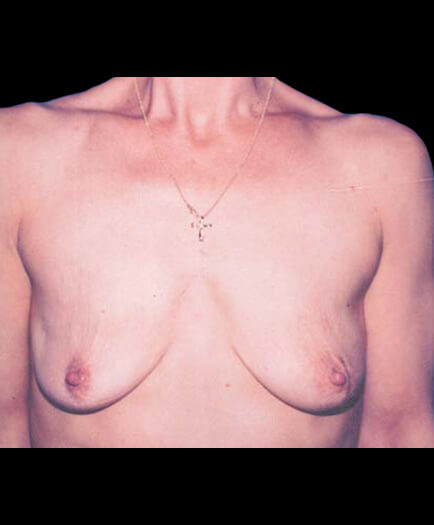
AFTER
Yes. In all cosmetic and reconstructive cases, medical photos are taken. Photographs are mandatory because this is the only way for us to compare your before and after results. Photographs in plastic surgery serve much the same role that x-rays serve for orthopedic surgery.
Dr. Marefat and the staff at Metropolitan Plastic Surgery would be happy to help you set up a private consultation to discuss breast reconstruction in Virginia. Schedule an appointment online or call one of our locations at 703-516-7600 (Arlington area) or at 703-560-9583 (Woodbridge).
Dr. Marefat offers a number of financial assistance programs and payment programs to cover the cost of breast reconstruction in Virginia. Please visit the patient financing section of our website for more details or ask the staff at Metropolitan Plastic Surgery about these options so that you can get started with breast reconstruction in Virginia today.